If perfected, the invention of synthetic and biomedically engineered corneas could have a major influence on the field of ophthalmology.
For patients suffering from severe corneal diseases, which can lead to blindness if left untreated, corneal transplants are considered an effective form of treatment. Corneal disease is one of the leading causes of blindness in the world and affects millions of people globally each year (Elisseeff, Madrid, Lu, Chae, & Guo, 2013). Research suggests that the number of corneal transplants needed each year will only grow as aging populations increase and donor cornea supplies decrease. In 2010, a study conducted in the Ukraine indicated that only 511 corneal transplants were performed despite the fact that 4,000 donor corneas were needed. The gap was caused by diminishing supplies of donor tissue and an increase in the number of cases involving transplant rejections, which occur when an individual’s immune system attacks and destroys the transplanted organ (Elisseeff, Madrid, Lu, Chae, & Guo, 2013). Luckily, the growing field of biomedical engineering provides endless possibilities for those who suffer from vision problems and corneal disease. Even now, many people, including my grandmother, are benefiting from the development of synthetic corneas.
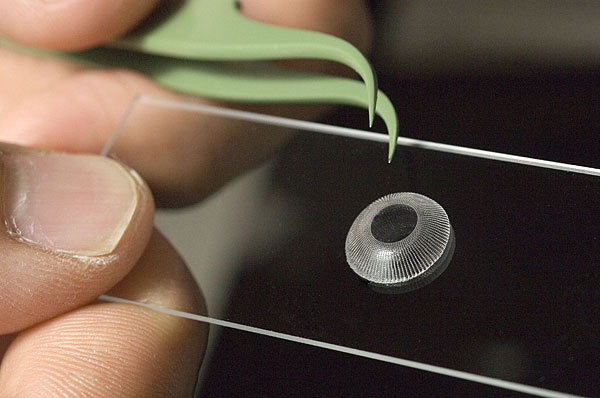
Synthetic keratoprosthesis, a procedure that replaces diseased corneas with artificial ones, may provide the first step towards this future. While there are various types of keratoprosthesis with differing designs and prognoses, most artificial corneas are made up of synthetic polymers or plastics fused with corneal tissue. According to many ophthalmologists, a type of keratoprosthesis, called the Boston KPro, is viewed as a gold standard for all other types of synthetic corneas, because a majority of people who receive Boston KPro transplants can noticeably see a difference in their quality of vision. Retention rates regarding the acceptance of the Boston KPro are also relatively high. One study suggests that the retention rates of the Boston KPro are typically 84 percent when examined over the course of about 17 months.
[Mohamed Fathy Oraby]. (2016, June 2). boston keratoprosthesis. [Video File]. Retrieved from https://www.youtube.com/watch?v=VGqh6aA_8CY
Nesta Ramazani, my 84-year-old grandmother, serves as further evidence that Boston KPro can drastically change one’s vision for the better. After my grandmother had four failed corneal transplants, she received a Boston KPro last March in hopes of restoring her vision. Before receiving the Boston KPro, my grandmother was practically blind in her right eye; now her vision is perfect in that eye. Additionally, my grandmother is less likely to need surgery in the future, because the chance of corneal rejection is lower in patients who receive the Boston KPro than patients who undergo corneal transplants (Ramazani, 2017).
While artificial corneas provide patients with many benefits, there are still many problems that must be addressed. According to my grandmother, she must return to the ophthalmologist’s frequently for check-ups, because problems with artificial corneas can advance more quickly than corneal transplants. She also has a permanent contact that can only be replaced by the ophthalmologists, which can be cumbersome when her vision becomes blurry due to the accumulation of particles, such as dust, on her contacts. Furthermore, most Boston KPro patients, including my grandmother, have to use multiple steroid and antibiotic eye drops each day (Ramazani, 2017). For these reasons, many ophthalmologists believe tissue-engineered corneas, rather than artificial corneas, would benefit people with corneal diseases more.
Cornea [Digital image]. (n.d.). Retrieved February 19, 2017, from http://www.corneatexas.com/cornea-disease
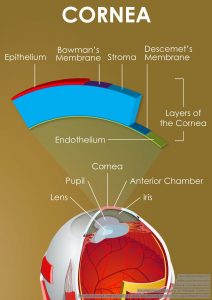
The importance of collagen regarding the construction of the cornea is evident in a recent study performed in the Ukraine, which gave three patients tissue engineered corneas comprised of collagen and synthetic phospholipids. All three of the patients were over fifty years old and were experiencing problems associated with corneal diseases, including pain and blindness. Two of the patients were experiencing problems due to burns, while the other patient was experiencing problems due to corneal rejection (Buznyk et al., 2015). According to the study, vision improved and pain and discomfort decreased in two of the three patients (Buznyk et al., 2015). These positive results indicate that tissue engineered corneas may be more effective than corneal transplants with regards to patients suffering from pathologies, such as burns, transplant rejection, and autoimmune disease. Additionally, a cost-minimization analysis was performed, suggesting that the production of tissue-engineered corneas is less expensive than donor corneas.
While more research needs to be done to create artificial eyes that can perfectly mirror the functionality of human eyes and to diminish the problems associated with artificial and tissue engineered corneas, my grandmother’s story provides hope for a future in which there are no more rejections.
References
Buznyk, O., Pasyechnikova, N., Islam, M. M., Iakymenko, S., Fagerholm, P. and Griffith, M. (2015), Bioengineered Corneas Grafted as Alternatives to Human Donor Corneas in Three High-Risk Patients. Clinical And Translational Science, 8: 558–562. doi:10.1111/cts.12293
Elisseeff, J., Madrid, M., Lu, Q., Chae, J., & Guo, Q. (2013). Future perspectives for regenerative medicine in ophthalmology. Middle East African Journal of Ophthalmology, 20(1), 38-45. doi:http://dx.doi.org/10.4103/0974-9233.106385
Giegengack, M., & Soker, S. (2013). Constructing the cornea: Hopes and challenges for regenerative medicine. Expert Review of Ophthalmology, 8(3), 209-211. doi:http://dx.doi.org/10.1586/eop.13.20
(N. Ramazani, personal communication, January 25, 2017).
Tan, T., Peh, G. S. L., George, B. L., Cajucom-Uy, H., Dong, D., Finkelstein, E. A., & Mehta, J. S. (2014). A cost-minimization analysis of tissue-engineered constructs for corneal endothelial transplantation. PLoS One, 9(6) doi:http://dx.doi.org/10.1371/journal.pone.0100563