Have you ever gone for a long run and said to yourself, “Wow, I feel so out of shape! My heart is beating like crazy!”? This is a daily struggle for people with damaged valves. The human heart is divided into four sections (called chambers), and each chamber has a valve that acts as a bridge for blood to enter and leave the heart to and from other parts of the body. When one valve is damaged, blood cannot flow into and out of the heart as effectively as it needs to, resulting in shortness in breath and an over-working heart.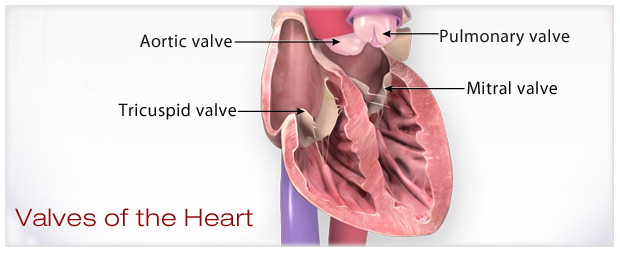
As years go on, the number of people with damaged heart-valves continues to increase. Heart-valve replacement surgeries are very common throughout the world; there are about 300,000 valve-replacement surgeries annually worldwide. Doctors have been unable to find the best way to perform this surgery that will give people the most favorable outcome post-surgery. Since the 1960s, around the time that heart valve-replacement surgeries began, the quest to find this “perfect” strategy has been far from easy. Doctors have attempted different strategies, and although none of them have been uniformly the best strategy for all patients, doctors continue to grow closer towards the most successful one.
The Quest for the Universal Strategy
Heart-valve replacement surgeries have tended to hurt the health of patients rather than improve health. For example, the most commonly used strategy for performing valve-replacements is not safe for most elderly patients. This strategy requires the work of a cardiopulmonary bypass machine (an instrument that takes over the job of the heart and lungs during surgery), which can place a lot of stress on a patient’s body. Elderly patients usually cannot undergo this surgery because of the amount of stress the surgery will place on them.
Younger patients are better suited for a different strategy, valve repair. The majority of younger patients have small tears in valves and do not need to go through a surgery that is very invasive to their body. Valve repair offers the option of repairing the valve torn rather than replacing it with an entirely new valve. While this is beneficial to younger patients, there are many older patients that have too large of tears in their valves which would make a valve-replacement the only option for them. Valve repair downsizes the number of eligible patients overall, making it a poor universal strategy. Since none of these surgery options are very compatible with the majority of the patient’s health, doctors began trying to place a small tube, called a catheter, which works on both younger and older patients. This strategy does not harm the body as much as previous strategies, and for the most part, this option is considered to be the best yet.
How Helpful is Medicine?
Another strategy that is intended to improve the life of patients with damaged valves is the use of medicine. Warfarin, for example, is an anticoagulant (an agent that can prohibit blood from clotting) used amongst the majority of patients in need of heart-valve replacement. When someone has a damaged valve, the healthy valves must compensate for the work the damaged valve loses. This can result in atrial fibrillation (a condition where the heart beats irregularly and quickly), and a common side effect of atrial fibrillation is blood clots. Patients use anticoagulants such as Warfarin to control their blood flow so that their blood doesn’t clump together and form a blood clot.
Although Warfarin is successful in controlling blood flow, major complications have risen from the use of Warfarin. Intracerebral hemorrhages (ICH), strokes that are caused when there is bleeding in the brain, have been linked to the use of warfarin and, in general, is a major side effect of anticoagulation. To develop a deeper understanding of the relationship between anticoagulants and conditions such as ICH, different studies have been conducted. One specific study observed the outcomes of patients with prosthetic valves that develop ICH’s.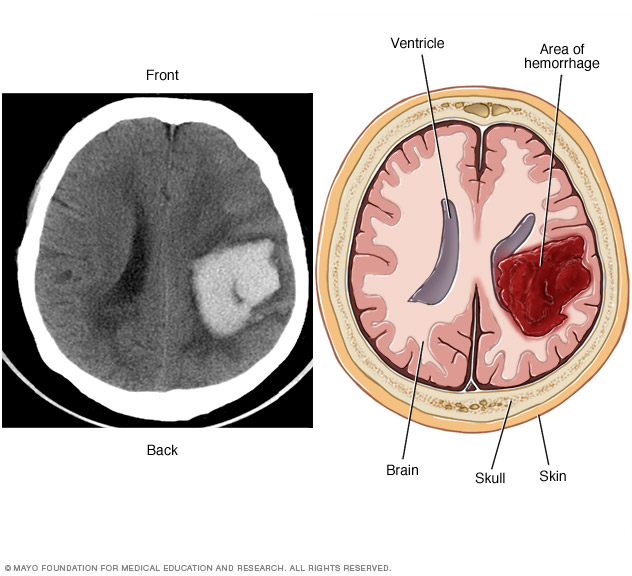
This computer-based study was based off of 38 patients with a prosthetic valve and ICH. Data was pulled randomly through the hospital’s database. Twenty-five of the patients had mechanical prosthetics valves and thirteen had bioprosthetic valves. Of these 38 patients, 31 of the patients were taking warfarin once admitted into the hospital. Results showed that eight patients of the 38 suffered hematoma enlargement, which is when the blood clot caused by ICH enlarges, four patients had an ischemic stroke (an obstruction in the blood vessel blocks blood, prohibiting the blood to get to brain), and three patients developed other hemorrhagic complications. Even though anticoagulation has proven to worsen the patient’s health, the patient must continue to use anticoagulation post ICH for his/her prosthetic valve. Without the continued use of anticoagulation, the risk of complications increases significantly.
Is there any Hope?
In the midst of searching for a universal strategy, a new issue became associated with strategies for performing heart-valve replacements. Doctors are now concerned with the fact that the prosthetic valve cannot grow with the patient as he/she grows. This greatly increases the risk of death for patients. Heart-valve replacement surgeries do not show preferable out-comes but rather complications that worsen the life-expectancy of the patient. The need for a more life-protecting surgery continues to increase, and some doctors believe one might be around the corner.
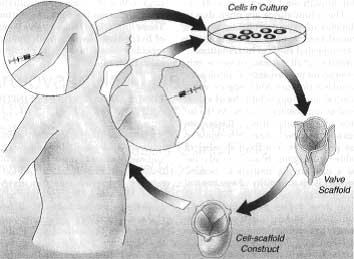
For about 30 years, scientists have created a different kind of prosthetic valve that can grow with the patient, and this invention has been improving each year. Tissue is used to create a prosthetic valve, often called TEHV (tissue engineered heart valve), and this tissue can regenerate and grow as the patient grows. Since TEHV is still fairly new, complications such as the valve degrading and the occurrence of inflammation arises frequently. As years of research continues, scientists have been able to practice using different materials that will help improve the quality of this tissue generating valve.
Currently, there are still many different things to be considered before releasing the TEHV strategy into the world for use. This prosthetic valve contains living cells, which makes it difficult to classify into a product group. The FDA and other regulating companies need to be able to produce regulations on this product before TEHV can be bought by biomedical companies. Also, for TEHV to be used regularly in practice, the handling/transportation, sterility, and overall care of the prosthetic valve must be improved. Although this new invention has not been tested enough to be approved for human surgery, this new strategy for heart-valve replacement surgery shows promise that will help about 300,000 worldwide live longer and healthier lives with their much healthier heart.